Posts tagged antiretroviral therapy

Mother-To-Child HIV Transmission Eliminated in Thailand
One of the biggest concerns in the world is the spread of HIV. This happens through unprotected sex, sharing needles, and more. Actions like these leave adults at risk. Unfortunately, the spread of HIV doesn’t stop with there. HIV transmission can happen during pregnancy, birth, or breastfeeding as well, causing an unborn child or infant to contract the disease. The World Health Organization (WHO) has made efforts to stop mother-to-child HIV transmission, and it has worked for Thailand.
Mother-To-Child HIV Transmission
Parents and soon to be mothers with HIV need to be aware that pregnancy, birth, and breastfeeding is the most common to spread the disease to your child. The CDC states these three facts:
- Approximately 8,500 women living with HIV give birth annually.
- Most (73%) of the estimated 174 children in the United States who were diagnosed with HIV in 2014 got HIV through perinatal transmission.
- Most (88%) of the estimated 104 children in the United States diagnosed with AIDS in 2014 got HIV through perinatal transmission.
In order to protect your child, it is important to be tested once you discover that you are pregnant. The risk of HIV significantly decreases to around 1 percent if HIV medicines are taken within the first 4-6 weeks.
How Thailand Has Eliminated This Transmission
Around the mid-1990’s, the rate of mother-to-infant HIV transmissions in Thailand was 20-40 percent. Using WHO’s recommended strategy, the government has successfully reduced transmissions to 1.9 percent. This strategy focuses on four areas of prevention and care:
- The prevention of HIV in women of childbearing age
- Stopping unintended pregnancies in women living with HIV
- The prevention of HIV transmission from an HIV-infected woman to her infant
- Provision of appropriate treatment, care, and support to women and children living with HIV
Thanks to the government’s initiative, they followed this strategy through the promotion of condoms, the distribution of HIV risk materials, and other efforts. Soon, more government money flowed into Thailand’s HIV/AIDS programs because of their successful efforts. Women have since had more access to HIV testing and antiretroviral therapy.
Awareness and determination like this spell a bright future for stopping HIV in its tracks.

Nanotechnology and HIV Drug Therapies
Nanotechnology sounds like science fiction. However, it is very real, and scientists are manipulating matter on an atomic, molecular, and supramolecular scale in order to achieve great things. One prime example is the development of HIV drug therapies. In a research study by the University of Liverpool, they sought to improve how HIV drugs are delivered to patients.
The Problem With HIV Drugs
HIV is a serious disease. It requires powerful medicine in order to combat its effects. Unfortunately, the drugs used to combat the virus need to be taken daily. This can be difficult for many patients. Keeping up with their regimen requires sticking to an intense schedule and remembering to take pills. Some even quit taking the drugs because of how demanding the therapy is.
With Solid Drug Nanoparticle (SDN) technology, scientists hope to improve HIV drugs. HIV patients want better drugs. Theoretically, this technology should make it easier for their bodies to absorb them. If successful, this form of nanotechnology would reduce the number or doses that HIV patients have to take, and possibly save them money.
Making Nanotechnology Applicable
Nanotechnology is still a relatively new field, which means that it is going to take some time to develop. Even worse, this type of medicine isn’t readily available to HIV patients. Currently, the University of Liverpool is developing a novel water dispersible nanotherapy for a poorly soluble antiretroviral medicine called lopinavir. It is still in the testing phase; however, some are hopeful of its success.
Research leader and Pharmacologist Professor Andrew Owen says “The fruits of our interdisciplinary research are beginning to be realized. Our approach has the potential to overcome challenges with current antiretroviral therapy, which include administration of high doses needed to achieve efficacious concentrations in the body, and the urgent need for better formulations for children living with HIV.”

90-90-90 Program: UNAIDS Treatment Plan for HIV
Research has uncovered information about HIV that has allowed progress to be made in the battle against this terrible disease. Vaccines and new approaches in medicinal therapies are being developed and tested. This process, as promising as it is, could take years before producing anything of use to the public. Despite these scientific breakthroughs, there are still pressing matters needing immediate attention. In an effort to address these matters, UNAIDS has move forward with a treatment plan called the “90-90-90” program might be implemented on a worldwide scale. But the 90-90-90 program has some obstacles to overcome—the largest one being the cost.
What Is the 90-90-90 Program?
The 90-90-90 program has three main objectives. First, to give a diagnosis to 90% of individuals with an HIV infection. The second goal is starting 90% of HIV-positive patients on antiretroviral therapy. The third objective is to have 90% of those on antiretroviral medications achieve viral suppression (making viral presence undetectable). The program has high aspirations that, if achieved, could mean a significant effect on the increasing number of new infections every year. Another byproduct of the program would be fewer children orphaned by the devastating effects of HIV and AIDS. It is hoped that with early detection and immediate treatment, more lives will be saved. The number of infections transmitted would be reduced as well if treatment was adhered to, and viral loads were sufficiently reduced.
Computer models have been used to help predict the results that this program would have over the next five to ten years. The 90-90-90 program would potentially prevent over 2 million new infections. Over 1.5 million children would not have to face the prospect of being orphaned. Millions of lives would be saved. What stands in the way of the program being set up around the world?
Money. The cost is very high, by some estimates over 40% more than what is currently being spent on similar efforts—bringing the total to $54 billion. Based on computer simulations, the program could be enough to bring the epidemic caused by HIV to an end. So while it would be an expensive venture, experts agree that the benefits would be worth it.

Enlightening Effect of Observing HIV Cellular Transmission
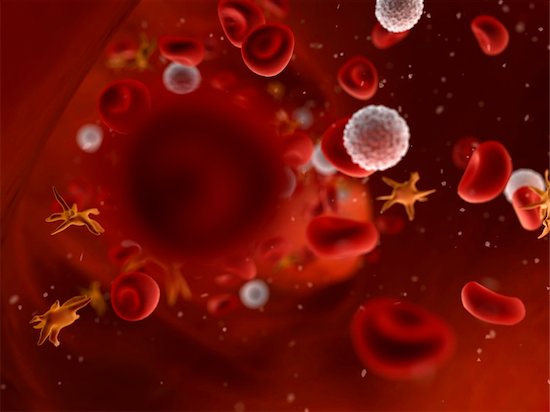
Scientists have discovered some interesting facts about the cellular transmission of HIV and how the virus moves throughout the body.
The inner workings of HIV, and the effectiveness with which it is able to transmit and spread infection, are complex. HIV cellular transmission has been carefully studied now for decades. The virus establishes itself in the host a couple of ways, and new information continues to be discovered. Cell-to-cell transmission has also been observed in the lab. Scientists have now been able to track HIV as it infects cells in real time in living organisms. This has big implications for the current approach to treatment and therapy.
Immune Cellular Transmission and the Role of Mutation
In this latest study, tracking HIV cellular transmission from cell to cell revealed a number of facts. First, the infected immune cell meets up with an uninfected cell, both being CD4 helper T cells. A sort of bridge is constructed between the two, and viral material that is passed along infects the second cell. The process, according to the researchers, is similar to the way nerve cells communicate information with each other. Cellular transmission works quickly. Several copies of the virus can pass through the bridge, making mutation easier. Mutant forms of the virus make it easy to escape detection from the immune system. This potent means of infection could prompt researchers to look to new approaches for treatment. Cell-to-cell transmission may increase resistance to antibodies, and the cells seem more resistant to current treatment options.
Today, antiretroviral therapies target viral particles floating in the bloodstream. It could be that cell-to-cell transmission takes place rapidly and goes undetected until the virus can be found in the blood. Reservoirs of infected cells are found in different tissues. Once infected, the immune cells can replicate, and clusters form rapidly. Treatments focusing on limiting or halting cell-to-cell transmission may be more effective at curbing the infection than current methods. Evidence that this could be useful if applied to potential vaccines was indicated as well.
In the U.S. alone, over one million people are living with HIV, and almost 40 million cases worldwide, so the search for effective treatments continues.
HIV Therapies According to Gender
The approach to treating HIV is similar for all—male and female, young and old. Adjustments can be made according to certain factors. A particular dosage may work for one, but may not be optimal for another. One recently published study shows why this can happen, and how medical professionals can increase the effectiveness of HIV therapies for their patients.
HIV Therapies and Gender
Preventing infection is an important part of curbing the spread of HIV. The drug used to prevent viral transfer is called Truvada. Until recently, it had been noted that the drug was most effective in men. Researchers found that it seemed less effective in women. Further investigation revealed that differences in tissues contributed to how well Truvada worked at preventing infection.
HIV needs access to genetic material in order to infect its host. The more DNA that is present, the stronger the viral hold. For women, vaginal and cervical tissues have more DNA present than in other types of tissue. Rectal tissue is also in this category. This requires considerable more medication to curtail HIV activity.
Armed with this knowledge, scientists mathematically calculated specific drugs-to-DNA ratios. Using this formula, and testing the outcomes, has proven successful. When increased doses were given to women, the rate of HIV infections decreased and more closely matched the male outcomes based on doses previously tried.
What does this mean for HIV therapies now? In short, women do best when taking Truvada every day. This contrasts considerably to the couple times a week generally prescribed. For the male population, the current dosage works well. Due to the anatomical differences, women require more of the medication. When taken daily, the rate of infection effectively decreases for this group. Of course, no one should change his or her therapy before consulting a healthcare provider.
So far, Truvada is the only FDA-approved pharmaceutical used to prevent the spread of HIV infections. Now with more information on how best to harness its potential, the medical world is in a good position to help keep others from contracting and spreading the virus.



