HIV

Factors to Consider When Working With HIV
As a result of better treatment options, more and more patients have considered finding employment and working with their HIV. As AIDSInfo states, many people living with HIV lead normal, healthy lives, including having a job. So, if you are healthy enough, and want to get back in the workforce after your HIV diagnosis, this is a possibility.
Seeking employment is a big step, though. Working with HIV has many benefits. However, many obstacles still stand in the way of many HIV-positive people seeking employment. For anyone living with HIV and looking to work, it’s important to consider these factors.
Working with HIV Has Positive Effects on Patients
When asked why they wanted to work, HIV-positive individuals cited a long list of reasons. Aside from the obvious financial benefits, a main driving force was that it increased their self-worth. For many people, what they do for a living is closely linked to how they perceive themselves. Being able to contribute in some way boosts their self-esteem.
Increased social interaction is another positive to working with HIV. Isolation is a common problem among people fighting HIV. Being around people every day creates a possibility for consistent engagement that would otherwise be harder to find.
Obstacles for HIV Patients in the Workforce
Research has found many concerns related to the possible loss of health benefits when re-entering the workforce. Depending on their healthcare plan, they may no longer be eligible to get those benefits.
They also fear the possibility of disclosure. Sensitive information of this ilk becoming public knowledge leads to worry about being discriminated against. Although there are laws in place to prevent this type of discrimination, it’s still a concern.
Working with HIV can provide financial independence and an improved sense of self-worth. But for many, the costs outweigh the benefits. Be sure to give each possibility a good amount of thought before deciding what’s best.

Enlightening Effect of Observing HIV Cellular Transmission
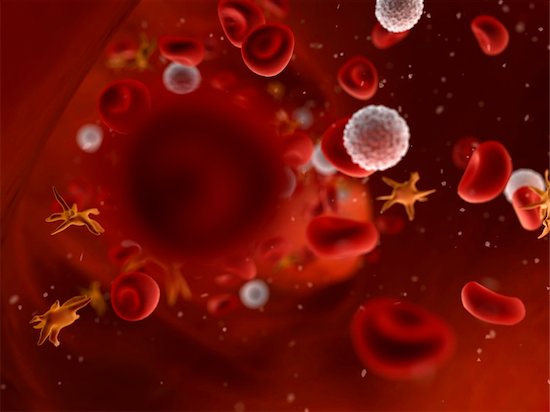
Scientists have discovered some interesting facts about the cellular transmission of HIV and how the virus moves throughout the body.
The inner workings of HIV, and the effectiveness with which it is able to transmit and spread infection, are complex. HIV cellular transmission has been carefully studied now for decades. The virus establishes itself in the host a couple of ways, and new information continues to be discovered. Cell-to-cell transmission has also been observed in the lab. Scientists have now been able to track HIV as it infects cells in real time in living organisms. This has big implications for the current approach to treatment and therapy.
Immune Cellular Transmission and the Role of Mutation
In this latest study, tracking HIV cellular transmission from cell to cell revealed a number of facts. First, the infected immune cell meets up with an uninfected cell, both being CD4 helper T cells. A sort of bridge is constructed between the two, and viral material that is passed along infects the second cell. The process, according to the researchers, is similar to the way nerve cells communicate information with each other. Cellular transmission works quickly. Several copies of the virus can pass through the bridge, making mutation easier. Mutant forms of the virus make it easy to escape detection from the immune system. This potent means of infection could prompt researchers to look to new approaches for treatment. Cell-to-cell transmission may increase resistance to antibodies, and the cells seem more resistant to current treatment options.
Today, antiretroviral therapies target viral particles floating in the bloodstream. It could be that cell-to-cell transmission takes place rapidly and goes undetected until the virus can be found in the blood. Reservoirs of infected cells are found in different tissues. Once infected, the immune cells can replicate, and clusters form rapidly. Treatments focusing on limiting or halting cell-to-cell transmission may be more effective at curbing the infection than current methods. Evidence that this could be useful if applied to potential vaccines was indicated as well.
In the U.S. alone, over one million people are living with HIV, and almost 40 million cases worldwide, so the search for effective treatments continues.
HIV Treatment Funding Is Out of Reach for Countries in Need
The battle against HIV has come a long way. Those living with the infection benefit from therapies now available. One of these benefits is a longer life expectancy. Worldwide, these implemented treatments not only improve quality and quantity of life, but it also limits the spread of the disease. Unfortunately, longer life equals more expense in lifetime treatment costs, which underdeveloped nations cannot support.
In spite of the good things being accomplished, the cost of maintaining what had been put into effect is already high and is increasing. Some of the countries hardest hit by HIV will experience the biggest cuts in funding. For these areas, future long-term care could be compromised. In Sub-Saharan Africa, home to some of the countries with the highest cases of HIV infections, studies were done to determine the cost of long-term therapy. The numbers are staggering. In order to maintain current treatment, account for new cases, and continue with prevention plans through the year 2050, it is estimated to cost over $260 billion. It’s a figure African countries simply can’t sustain.
Some Countries with the Greatest Need Have the Least Resources
The areas that were investigated are the ones that account for well over two-thirds of HIV infections in all of Africa. These nations do not have the resources to continue to provide necessary and ongoing care for HIV patients. Experts feel it’s vital to collect the needed funding now to ensure it is there for the future. Otherwise, lack of funds for treatment could lead to an increased prevalence of AIDS, as well as an increase in the spread of HIV.
As previously mentioned, long-term care is important for each individual who is HIV-positive. Part of the treatments include inhibiting the transfer of the virus. Stopping the spread of the disease is vital. Researchers emphasized the need for continued support in the fight against HIV, not only for the financial reasons but the moral ones as well. With so many people able to have a relatively healthy and normal life because of current plans in place, their lives are dependent on continued care and the funding that backs it.
Immune Exhaustion and HIV
HIV infection has long been known to cause immune exhaustion. Even with current therapies, this is a chronic issue. Finding ways to lessen the burden on the immune system, while still keeping the virus at bay, have been studied. Recently, some new experimental treatments have brought to light some interesting conclusions on the matter. It is hoped that the information thus gathered will help control the problem for many in the near future.
What the Research Reveals About Immune Exhaustion
Delicate balances keep everything in existence – from the largest systems to the smallest organisms. The interactions between the medications that keep the HIV counts low, the immune T cells, and the proteins that signal immune exhaustion are extremely precise and particularly balanced. Researchers have studied the effects of blocking the protein pathways, which are known to signal the exhaustion. In doing so, they have discovered that people can recover from immune exhaustion. However, a number of things must be in place for this to happen.
The exhausted T cells are the ones that have the protein, PD-1, which signals the exhaustion. The partner to that protein binds to it, and this is how researchers can identify the exhausted cell. By blocking the path between these two proteins, the immune system has a chance to regain normal function.
A Very Specific Process
When tested, this strategy was effective, but only under specific circumstances. First, if viral levels in the blood were high, adding the protein blockade actually increased viral production. Best results were yielded when the viral load was low. Also important is how the T cells react, as their numbers also increase. However, with low viral load and cooperating immune cells, restoring a measure of strength back to the immune system is possible with this method.
Further testing is underway, as are trials to see just how effective this approach can be. Of course, if implemented in the future, patient screening will be necessary. In the meantime, antiretroviral therapies continue to be an important part of both managing viral count and slowing disease progression.
Potential Key to a Cure for HIV
Antiretroviral therapies are efficient at lowering HIV levels in the blood. They suppress these levels enough that the virus can become virtually undetectable, making it hard to cure. While this provides the patient with a measure of health, and also slows disease progression, it is not enough to completely eradicate the virus from the body. Why is this the case? What is the key to eliminating the tenacious invader completely so as to have a cure?
Progress Towards a Cure
Study after study continues to show that antiretroviral therapy alone cannot completely rid the body of HIV. It is true that low viral levels within the blood can prove lifesaving, but HIV finds a way to hide, replicate, and even thrive. Attempting to kill off the virus in these areas is the key to completely wiping it out. Blood levels can be kept low because the drugs can effectively work within the vascular network. Researchers are finding that stores of HIV are located within the lymphatic system, specifically in lymph nodes and like tissues.
This presents challenges for healthcare. One, it is difficult for pharmaceuticals to reach the specific tissues where the virus replicates. It is rare for medications to filter into these lymph nodes. Also, there is the matter of viral mutation. As HIV patients increase in numbers, changes in the disease’s resistance to drugs begins to appear.
The good news is that usually it is the non-resistant form of the virus that hides and replicates. Once it releases into the blood, the drug therapies are still effective. Also, when researchers exposed the infected tissues to the drugs, the infection could be cleared. However, depending on the type and concentration of the drug therapy, the amount of drug-resistant HIV can fluctuate, making things complicated.
Further investigation is underway about how to infiltrate lymphatic tissue in order to remove stores of HIV. Researchers are convinced that once they gain a better understanding of how to reach these areas—combined with antiretroviral therapies—a cure for HIV will be at hand. Until then, daily treatment is the only way to keep the disease from progressing.

