Posts tagged HIV breakthrough

New HIV Antibodies Created to Fight Off the Virus
Scientists have made a huge step towards fighting off the HIV virus. Researchers at The Scripps Research Institute (TSRI) were able to attach HIV antibodies to immune cells in their most recent study. These new cells could potentially be the cure that millions infected with the life-threatening disease need. Find out what the scientists at TSRI had to say about their research and how these new cells eliminate the virus from the body.
How Do the HIV Antibodies Work?
Typically, antibodies float in the bloodstream alongside the cells in the body. However, the HIV antibodies developed by the researchers work a little differently. The scientists were able to tether the antibodies to immune cells. This technique created a new population of resistant cells that can replace cells affected by the disease.
This close connection with the immune cells is what Jia Xie, a senior staff scientist at TSRI and first author of the study, called the “neighbor effect.” Essentially, the antibodies hang on to a cell’s surface, acting as a barrier between HIV and the cell’s receptor. This action prevents HIV from infecting the cells and spreading throughout the body.
“This protection would be long term,” said Jia Xie. “You don’t need to have so many molecules on one cell to be effective,” he said.
How Was the Test Preformed?
Xie and his researchers first tested the tethering system against the rhinovirus, which is otherwise known as the common cold. The researchers were able to apply a new gene to cultured human cells. This gene is the one responsible for the creation of the antibodies that attached to immune cells.
The antibodies protected the cell receptors from the virus, halting infection. When adding rhinovirus to the testing, many of the unprotected cells died off. However, the newly created antibodies were able to thrive as the number of cell populations recovered to almost normal levels.
The next step after this success was to test the antibodies against HIV. The goal was for the HIV antibodies to protect the CD4 cells, which are usually the target of HIV. In the end, an HIV-resistant population of cells grew, while the old cells died. This is exactly the type of success that the team at TSRI was looking for.
What This Means for the Future
Antiretroviral drugs are the primary defense against HIV. The problem with this type of medication is that they have to be taken daily. Sometimes, HIV-positive individuals still suffer from higher rates of diseases when taking the drugs.
When discussing the TSRI’s research and new techniques, Joseph Alvarnas, M.D., director of Value-Based Analytics at the City of Hope, states “HIV is treatable but not curable–this remains a disease that causes a lot of suffering. That makes the case for why these technologies are so important.”
The research still has a long way to go. Scientists are testing to find out what other parts of the cell the new antibodies can protect. Hopefully, this can lead to a potential cure.

Early HIV Intervention Helps Manage HIV-Like Virus
Nothing is more important than getting tested for HIV as soon as possible. If you test positive, an early diagnosis can increase your chances of managing the virus. Early HIV intervention is a crucial step in protecting your health. HIV can be a tricky disease that likes to hide. This makes the virus difficult to treat before it attacks the immune system.
In a study to better control the disease’s progression within the body, the Rockefeller University tested and treated monkeys infected with an HIV-like virus. Find out the results of their research and what this could mean for patients with HIV.
New Form of HIV Therapy
The Rockefeller University and the National Institute of Health wanted to find a way to tackle HIV while it lays dormant within the body. The virus often hides like this to avoid being eradicated. It waits for the perfect opportunity, like when treatment is interrupted, to attack the immune system.
Using macaque monkeys and a model of HIV, the researchers were able to simulate the effects of the HIV virus in humans. 13 monkeys were tested over a two-week period of they were injected with the virus. While the model, which is known as the simian-human immunodeficiency (SHIV), is not a 1 to 1 recreation of the virus, it helps explore ways to control the virus.
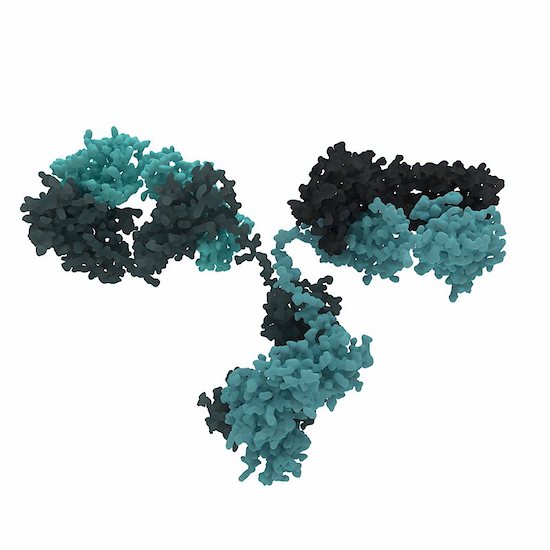
The new treatment uses two anti-HIV antibodies to give a boost to the immune system. These antibodies were discovered in individuals with a rare ability to fight the infection. New drugs (3BNC117 and 10-1074) were developed and they enable the body to take control of the virus and hold off its effect for a long period of time. However, the researchers suggest that this all works because the treatment was given soon after infection.
“This form of therapy can induce potent immunity to HIV, allowing the host to control the infection,” says Michel Nussenzweig, head of the Laboratory of Molecular Immunology and an Investigator with the Howard Hughes Medical Institute. “It works by taking advantage of the immune system’s natural defenses, similar to what happens in some forms of cancer immunotherapy.”
The Success of Early HIV Intervention
The monkeys showed significant improvement after taking the new drugs. After treatment was initially given, HIV levels dropped until they were nearly undetectable. The positive progress of the subjects continued 5 to 22 months later as the monkey regained control of the virus. The virus then dropped again and stay at low levels for another 5 to 13 months.
Further studies need to be done to see if this treatment is feasible in humans. During the study, the scientists also investigated cytotoxic T cells. When they decreased these cells in the monkeys’ bodies, SHIV levels increased. It proved that these cells may have helped the monkeys fight off the virus.
Their next test is to see if the drugs are still effective after long-term infection and without early HIV intervention. They are going to have the monkey exposed to the virus for about two to six weeks before treating them. Hopefully, the results will remain positive.

Nanotechnology May Improve HIV Medicines
Scientists and researchers focus on the improvement of HIV medicines in order to one day find a cure for the virus. Another reason the medical society puts so much effort into better medicine is to improve the lives of patients. In a new trial, the University of Liverpool has found success in using nanomedicine to potentially reduce the dosage of HIV treatment.
Using Nanotechnology for HIV Medicines
Nanotechnology is the process of making things on a smaller scale. That requires the manipulation of matter on the atomic, molecular, and supramolecular level. In nanomedicine, this means smaller, less expensive pills that work more effectively. This technology can change the way that future medicine is made.
The University of Liverpool’s Success
Both doctors and patients alike are hopeful for nanomedicine’s success. The University of Liverpool led a trial to prove the benefits of this type of medicine, with the intent to promote its usage within the scientific community.
The results from their trial showed that nanomedicine is far more effective. The body is able to absorb more of the drug. This means that patients can receive the same quality treatment and reduce the number of dosages they take. In fact, they found that patients could take potentially take half of the dosage and fight off the disease.
Today’s HIV therapies require daily doses just to keep up with the virus. This medicine can save HIV-positive individuals a significant amount of money on treatment. In certain countries where HIV is prevalent, this could mean better access to treatment by making the drugs more affordable.
Nanomedicine may also prevent non-adherence to therapy, which happens often when patients undergo the strain of taking medications daily. If the success of this trial can influence future HIV medicine, then this might prove great news for patients fighting against the virus. Hopefully, more research can lead to the technology’s implementation.

New HIV Neutralizing Antibody Proves Successful
It is always good news when scientists make brand-new developments in HIV research. Breakthrough information helps scientists and doctors create new medicine and therapies for patients. A recent study from the Rockefeller University in New York and Prof Florian Klein, University Hospital Cologne and German Center for Infection Research (DZIF) has found an HIV neutralizing antibody effective against an HIV strains.
10-1074: The HIV Neutralizing Antibody
Scientists are optimistic about the newest generation of HIV neutralizing antibodies. Prof. Florian Klein and his team decided to test one of these antibodies. They wanted to find out if it could be used to treat the disease.
Prof. Klein states “These antibodies are highly potent and are able to effectively neutralize a large number of different HIV strains. Therefore, they play an important role in the quest for and development of an HIV vaccine.”
The 10-1074 antibody targets a certain structure on the HIV envelope protein. The antibody proved effect as a drug and antibody during testing. The results of this research saw a high antiviral activity within patients who have HIV.
Positive News
Through the collaborative work among the three institutions, this is positive news for patients with HIV. They are already looking at how the virus escapes most antibodies.
“We performed a comprehensive HIV sequence analysis to investigate the dynamics and mechanisms HIV uses to escape the selection pressure by the antibody,” says Dr. Henning Gruell, one of the first authors of the current publication.
HIV is still a troubling disease. By the end of 2015, there were 2.1 million newly infection patients with HIV and 36.7 million people living with the virus. More than 18.2 million are prescribed antiretroviral therapy. These numbers are startling.
The most important thing anyone can do in the fight against HIV is get tested. Knowing your status helps you take the rights steps to protect your health. Visit an HIV doctor today.

HIV Breakthrough Deciphers the Structure of the Virus
There is one question that has eluded scientists for so many years. How does HIV integrate into human host DNA and replicate in the body? More than a decade later, researchers have found the answer. An HIV breakthrough at the Salk Institute has deciphered the structure of HIV machinery.
Intasome: The Machinery Making Trouble
HIV intasome is a large molecular machine that adds viral DNA into the genomes of its host. This machinery is responsible for HIV’s elusive nature and its ability to hide within the body.
According to Dmitry Lyumkis, senior author, and fellow at the Salk Institute: “HIV is a clever virus and has learned to evade even some of the best drugs on the market. Understanding the mechanisms of viral escape and developing more broadly applicable drugs will be a major direction in the future.”
Scientists have come up with a way to combat intasome before by using a drug called integrase strand transfer inhibitors (INSTIs). It is approved to treat the virus in both the U.S. and Europe. However, the drugs and HIV machinery are a bit of a conundrum. Without being able to study intasome on the atomic level, the drug’s effects are not as powerful as it should be, leaving scientist stumped on how it should work.
How This HIV Breakthrough Was Made
New technology allows us to do better things. The same is true within the scientific community. The state-of-the-art imaging technique called the single-particle cryo-electron microscopy (cryo-EM) gave researchers the ability to image large, complex and dynamic molecules. Basically, they were able to see intasome structure clearly.
The molecular machine is composed of a four-part core but has many other complex parts to it. The researchers believe that this allows it to gain access to the cell’s nucleus through active transport instead of waiting for the cell to divide. Lyumkis calls for understanding each of these parts a bit more to combat the disease.