Posts tagged HIV

Eliminating HIV in Sub-Saharan Africa Proves Difficult
We’ve discussed HIV’s impact on the sub-Saharan region of Africa before. Over the years, the disease has infected more than 25 million people, with the number of new infections rising every year. One the biggest obstacles the area faces is a lack of access to condoms. This contraceptive is rarely used among men and women in these countries. Eliminating HIV is no easy task, especially in a region where the prevalence of HIV is 1.5 times higher than Europe and the United States. The UN’s latest efforts to reduce the spread of the disease seems likely to fail.
Eliminating HIV in This Region Isn’t Easy
Organizations like the World Health Organization (WHO) and UNAIDS have found success in reducing the number of HIV patients in the United States and other similar countries. However, those countries are resource-rich areas, where they have the means and money to educate and distribute HIV protection. Both organizations have tried to implement similar efforts in the sub-Saharan region.
WHO and UNAIDS sought to use treatment as a prevention method. The plan would treat HIV-positive individuals and reduce their ability to infect others. They hoped to diagnose and treat 90 percent of the people within the next three years.
Why Researchers Cast Doubt
Unfortunately, a study by UCLA researchers cast doubt on this plan, seeing it as unfeasible. The researchers used statistical mapping to find people infected with HIV in Lesotho. At least 1 in 4 people have HIV in this South African country. Similar to other South African countries, most people have gone without a diagnosis, nor are they receiving treatment. The scientists discovered that the plan couldn’t address the fact that HIV-positive individuals are widely dispersed within the country. Also, very little of the population lives in urban areas, making it hard to find these people.
“Global health policies for HIV elimination need to be redesigned, and they need to consider settlement patterns and population density,” said Sally Blower, director of UCLA’s Center for Biomedical Modeling. “Our results show that the spatial demographics of populations in predominantly rural countries in sub-Saharan Africa will significantly hinder, and may even prevent, the elimination of HIV.”
“We estimate that almost every settlement in the country has at least one HIV-infected person, and this holds true for even the smallest and most remote settlement,” said Brian Coburn, the study’s other co-author, who was a postdoctoral fellow in Blower’s group. “We also found that approximately 70 percent of HIV-infected adults live in rural settlements.”
With those in need of treatment so widespread, it becomes harder and more expensive to help them. For every rural location, there is an average of two or fewer people per square kilometer who is HIV-positive. The problem is reaching them.
The Importance of Finding a Great Plan
The researchers at UCLA are using their technology to find alternate plans that address these issues. Blower states that in order “To develop effective strategies, we need to figure out — throughout entire countries — where HIV-infected individuals live and which communities are connected to each other.” Hopefully, whatever plan the governments of Africa chooses can curb the epidemic plaguing the continent and eventually help in eliminating HIV.

The Sneaky Nature of the HIV Virus
There is no doubt that HIV is a deadly virus. Since it was discovered, this pandemic has infected 78 million people and 35 million have died due to an AIDS-related illness. The worst part is that scientists have yet to find an absolute cure to the disease. Why is it that the HIV virus is so hard to eradicate? What is it about the disease that makes treatment difficult?
Many experts note the infection’s ability to hide within the body. HIV is notorious for eluding even the most powerful combinations of medicine. The sneaky nature of the disease allows it to wait until the right moment, when the body’s defenses are down, to attack the immune system. Even today, scientists are still trying to figure out and understand exactly how the virus works in order to combat its effects on the body.
How the HIV Virus Moves Within the Body
Once the body is infected with HIV, the virus begins to attack the immune system. It’s number one target are the CD4 cells in the body. These cells help the immune system fight off infection and diseases. Little by little, HIV lowers the CD4 count until the body can no longer protect itself.
The best defense against HIV is antiretroviral therapy (ART). This is a combination of several medications that work together to suppress HIV levels in the body. In order for this treatment to work, it has to be taken daily. When taken properly, the treatment has proven effective in reducing traces of the virus to nearly undetectable levels and preventing the progression of the disease to aids.
What Studies Have Found
ART is no cure. Traces of the virus remain within the body despite the use of these strong medications. The virus likes to hide in immune cells when at low levels. By remaining dormant in these “Sanctuary Sites,” it can wait in places unreachable by drugs. Once it has found the right moment, it will quickly reproduce when an HIV positive individual stops taking ART therapy.
In a recent joint study by the Monash Biomedicine Discovery Institute and the Systems Immunity Research Institute at Cardiff University, the two institutions discovered that mutations within HIV help it appear dormant and virtually undetectable by the immune system. These mutations change the way that key immune molecules called Major Histocompatibility Complex (MHC), display the virus.
“This work uncovers a novel mechanism for HIV immune escape, which will be important to incorporate into future vaccine development and may have broader implications for immune recognition of MHC molecules,” he said.
What You Can Do
While scientists work hard to find a way to detect and eradicate the HIV virus completely, you have to do your part to curb the spread of the virus. Protect by getting tested. Knowing is an important step. If you are HIV-negative, protect yourself by practicing safe sex and taking pre-exposure prophylaxis (PrEP). For those infected by the disease, remember to take ART daily to prevent the virus from progressing.

Early HIV Intervention Helps Manage HIV-Like Virus
Nothing is more important than getting tested for HIV as soon as possible. If you test positive, an early diagnosis can increase your chances of managing the virus. Early HIV intervention is a crucial step in protecting your health. HIV can be a tricky disease that likes to hide. This makes the virus difficult to treat before it attacks the immune system.
In a study to better control the disease’s progression within the body, the Rockefeller University tested and treated monkeys infected with an HIV-like virus. Find out the results of their research and what this could mean for patients with HIV.
New Form of HIV Therapy
The Rockefeller University and the National Institute of Health wanted to find a way to tackle HIV while it lays dormant within the body. The virus often hides like this to avoid being eradicated. It waits for the perfect opportunity, like when treatment is interrupted, to attack the immune system.
Using macaque monkeys and a model of HIV, the researchers were able to simulate the effects of the HIV virus in humans. 13 monkeys were tested over a two-week period of they were injected with the virus. While the model, which is known as the simian-human immunodeficiency (SHIV), is not a 1 to 1 recreation of the virus, it helps explore ways to control the virus.
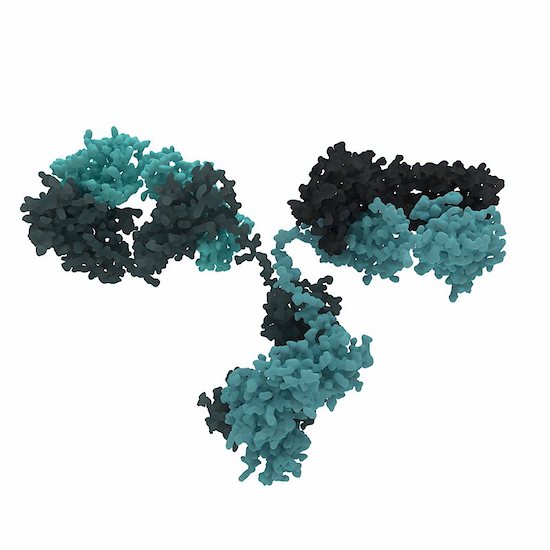
The new treatment uses two anti-HIV antibodies to give a boost to the immune system. These antibodies were discovered in individuals with a rare ability to fight the infection. New drugs (3BNC117 and 10-1074) were developed and they enable the body to take control of the virus and hold off its effect for a long period of time. However, the researchers suggest that this all works because the treatment was given soon after infection.
“This form of therapy can induce potent immunity to HIV, allowing the host to control the infection,” says Michel Nussenzweig, head of the Laboratory of Molecular Immunology and an Investigator with the Howard Hughes Medical Institute. “It works by taking advantage of the immune system’s natural defenses, similar to what happens in some forms of cancer immunotherapy.”
The Success of Early HIV Intervention
The monkeys showed significant improvement after taking the new drugs. After treatment was initially given, HIV levels dropped until they were nearly undetectable. The positive progress of the subjects continued 5 to 22 months later as the monkey regained control of the virus. The virus then dropped again and stay at low levels for another 5 to 13 months.
Further studies need to be done to see if this treatment is feasible in humans. During the study, the scientists also investigated cytotoxic T cells. When they decreased these cells in the monkeys’ bodies, SHIV levels increased. It proved that these cells may have helped the monkeys fight off the virus.
Their next test is to see if the drugs are still effective after long-term infection and without early HIV intervention. They are going to have the monkey exposed to the virus for about two to six weeks before treating them. Hopefully, the results will remain positive.

New HIV Neutralizing Antibody Proves Successful
It is always good news when scientists make brand-new developments in HIV research. Breakthrough information helps scientists and doctors create new medicine and therapies for patients. A recent study from the Rockefeller University in New York and Prof Florian Klein, University Hospital Cologne and German Center for Infection Research (DZIF) has found an HIV neutralizing antibody effective against an HIV strains.
10-1074: The HIV Neutralizing Antibody
Scientists are optimistic about the newest generation of HIV neutralizing antibodies. Prof. Florian Klein and his team decided to test one of these antibodies. They wanted to find out if it could be used to treat the disease.
Prof. Klein states “These antibodies are highly potent and are able to effectively neutralize a large number of different HIV strains. Therefore, they play an important role in the quest for and development of an HIV vaccine.”
The 10-1074 antibody targets a certain structure on the HIV envelope protein. The antibody proved effect as a drug and antibody during testing. The results of this research saw a high antiviral activity within patients who have HIV.
Positive News
Through the collaborative work among the three institutions, this is positive news for patients with HIV. They are already looking at how the virus escapes most antibodies.
“We performed a comprehensive HIV sequence analysis to investigate the dynamics and mechanisms HIV uses to escape the selection pressure by the antibody,” says Dr. Henning Gruell, one of the first authors of the current publication.
HIV is still a troubling disease. By the end of 2015, there were 2.1 million newly infection patients with HIV and 36.7 million people living with the virus. More than 18.2 million are prescribed antiretroviral therapy. These numbers are startling.
The most important thing anyone can do in the fight against HIV is get tested. Knowing your status helps you take the rights steps to protect your health. Visit an HIV doctor today.

The Consequences of HIV Being Stigmatized
Prevention starts with making HIV less stigmatized. Since its initial outbreak in the 1980s, this has been a major issue. While there is a complexity to this, it’s necessary to address. Getting rid of the lingering stigma will prove to benefit those living with HIV. Over the years, many studies have shown this. Two sectors where a change in procedure would benefit HIV patients most is among health care and law enforcement officials.
HIV Patients Stigmatized by Health Care Providers
Whether it’s intentional or not, HIV inhibits far too many people from accessing HIV prevention, testing, and care, even today. According to the World Health Organization, health workers in several countries have committed breaches of confidentiality.
Honesty is important in these situations. Lack of discretion limits how honest patients are. Fear is another consequence. Less testing is a result of fear. The possibility of that information being made known against their will is a big problem.
HIV Patients Stigmatized by Laws
Criminalizing HIV is another way in which the disease remains stigmatized. They have little basis. There’s very little evidence that they’ve effectively reduced HIV. Up to a quarter of these cases involve either a low or no-risk activity.
Many believe that these laws can undermine prevention efforts. If afraid, testing for HIV among people at risk will be less common. Also, laws of this nature create widespread confusion about which activities are considered high risk. People must be properly educated on HIV in order to prevent it.
Taking preventative measures in making HIV less stigmatized leads to better HIV prevention in general. Better laws could lead to better education. And training health care providers to be better equipped at handling such a sensitive situation would do wonders. Do not underestimate these factors. They can make a difference.