Nanotechnology May Improve HIV Medicines
Scientists and researchers focus on the improvement of HIV medicines in order to one day find a cure for the virus. Another reason the medical society puts so much effort into better medicine is to improve the lives of patients. In a new trial, the University of Liverpool has found success in using nanomedicine to potentially reduce the dosage of HIV treatment.
Using Nanotechnology for HIV Medicines
Nanotechnology is the process of making things on a smaller scale. That requires the manipulation of matter on the atomic, molecular, and supramolecular level. In nanomedicine, this means smaller, less expensive pills that work more effectively. This technology can change the way that future medicine is made.
The University of Liverpool’s Success
Both doctors and patients alike are hopeful for nanomedicine’s success. The University of Liverpool led a trial to prove the benefits of this type of medicine, with the intent to promote its usage within the scientific community.
The results from their trial showed that nanomedicine is far more effective. The body is able to absorb more of the drug. This means that patients can receive the same quality treatment and reduce the number of dosages they take. In fact, they found that patients could take potentially take half of the dosage and fight off the disease.
Today’s HIV therapies require daily doses just to keep up with the virus. This medicine can save HIV-positive individuals a significant amount of money on treatment. In certain countries where HIV is prevalent, this could mean better access to treatment by making the drugs more affordable.
Nanomedicine may also prevent non-adherence to therapy, which happens often when patients undergo the strain of taking medications daily. If the success of this trial can influence future HIV medicine, then this might prove great news for patients fighting against the virus. Hopefully, more research can lead to the technology’s implementation.

Better HIV Treatment Leads to Riskier Behavior in Gay Men
The advancements in HIV treatment have made it easier to stall the progression of the virus. However, a new study suggests that the news of these treatments is having an unintended consequence. More gay men are engaging in risky behavior because they believe that antiretroviral medicines will keep them safe. However, the continuation this kind of behavior only increases their risk despite taking proper prevention methods.
The Risk to Gay Men
Gay Men are already more likely to contract HIV than others. In 2015, gay and bisexual men accounted for 67 percent of all new diagnoses. Anal sex is the highest risk factor for HIV transmission. Receptive anal sex puts more men at risk than insertive anal sex. This is because of the rectums thin lining, which allows HIV to enter the body more easily. The transmission of HIV can happen from semen or pre-seminal fluid.
The Danger of Relying Solely on Medicinal HIV Treatment
Study leader Seth Kalichman of the University of Connecticut and his team analyzed a survey spanning 19 years. Participants at a gay pride event noted their sexual habits. Here is what they found:
- An increase in condomless sex among men.
- A rise in the number of sexual partners that men engaged with.
- Condomless receptive anal sex has doubled in HIV-negative men.
- Condomless insertive anal sex has tripled in HIV-negative men.
We are seeing a considerable increase in unsafe sex because gay men perceive antiretroviral drugs to be enough. However, after looking at the survey data, they found there wasn’t much of a reduction of new HIV infections in major cities. In fact, certain countries with HIV testing programs and antiretroviral drugs have seen infection grow among gay men. The risk remains when unsafe behavior increases.
Kalichman concludes that “The current study adds to the mounting evidence that substantial changes have occurred in community-held beliefs that condomless anal sex is safer in the era of HIV treatment as prevention.”

Mother-To-Child HIV Transmission Eliminated in Thailand
One of the biggest concerns in the world is the spread of HIV. This happens through unprotected sex, sharing needles, and more. Actions like these leave adults at risk. Unfortunately, the spread of HIV doesn’t stop with there. HIV transmission can happen during pregnancy, birth, or breastfeeding as well, causing an unborn child or infant to contract the disease. The World Health Organization (WHO) has made efforts to stop mother-to-child HIV transmission, and it has worked for Thailand.
Mother-To-Child HIV Transmission
Parents and soon to be mothers with HIV need to be aware that pregnancy, birth, and breastfeeding is the most common to spread the disease to your child. The CDC states these three facts:
- Approximately 8,500 women living with HIV give birth annually.
- Most (73%) of the estimated 174 children in the United States who were diagnosed with HIV in 2014 got HIV through perinatal transmission.
- Most (88%) of the estimated 104 children in the United States diagnosed with AIDS in 2014 got HIV through perinatal transmission.
In order to protect your child, it is important to be tested once you discover that you are pregnant. The risk of HIV significantly decreases to around 1 percent if HIV medicines are taken within the first 4-6 weeks.
How Thailand Has Eliminated This Transmission
Around the mid-1990’s, the rate of mother-to-infant HIV transmissions in Thailand was 20-40 percent. Using WHO’s recommended strategy, the government has successfully reduced transmissions to 1.9 percent. This strategy focuses on four areas of prevention and care:
- The prevention of HIV in women of childbearing age
- Stopping unintended pregnancies in women living with HIV
- The prevention of HIV transmission from an HIV-infected woman to her infant
- Provision of appropriate treatment, care, and support to women and children living with HIV
Thanks to the government’s initiative, they followed this strategy through the promotion of condoms, the distribution of HIV risk materials, and other efforts. Soon, more government money flowed into Thailand’s HIV/AIDS programs because of their successful efforts. Women have since had more access to HIV testing and antiretroviral therapy.
Awareness and determination like this spell a bright future for stopping HIV in its tracks.

Diabetes Risk: HIV Patients Have a Higher Risk
Patients with HIV are always at risk. They are left vulnerable to infections and other comorbidities due to the virus attacking their immune system. Scientists were startled when they made the revelation that HIV patients had a 4 percent higher risk of developing diabetes. This discovery was made in a recent study published in the BMJ Open Diabetes Research & Care online journal.
Despite Low Obesity Rates, Diabetes Risk Persist
Obesity is a key indicator of diabetes. However, many patients with HIV do not have obesity, a fact leaving scientist confused. To find out just how prevalent diabetes is among the HIV population, researchers launched a probe into two sets of data from 2009-2010.
They analyzed a survey of 8,610 HIV-positive individuals in the Medical Monitoring Project (MMP) and another survey of 5,064 people without the disease who participated in the annual National Health and Nutrition Examination Survey (NHANES). Comparing these two sets of data would give them insights into the diabetes risk of those with and without HIV.
Here is the breakdown of what the researchers found:
- One in 10 HIV patients had diabetes.
- 4% of those with diabetes had type 1.
- Over of those with diabetes had type 2.
- 44% of HIV patients had and unspecified strain.
- Over 8% of the general population had diabetes.
- The occurrence of diabetes was 3.8% higher in HIV patients.
This study was able to show that HIV patients are at risk. However, since the research was purely observational, scientists were not able to make a definitive conclusion as to why. They know that obesity is still a risk factor, but due to its high absence in individuals with HIV, they have to think differently.
The researchers had this to say: “Additional research would help to determine whether [diabetes] screening guidelines should be modified to include HIV infection as a risk factor for [the condition], and to identify optimal management strategies in this population.”

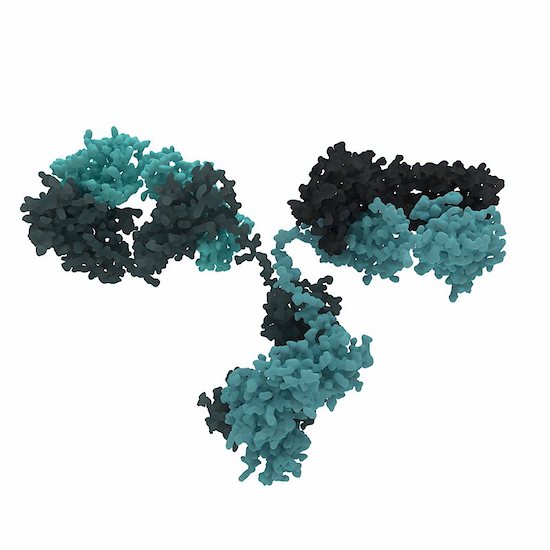
New HIV Neutralizing Antibody Proves Successful
It is always good news when scientists make brand-new developments in HIV research. Breakthrough information helps scientists and doctors create new medicine and therapies for patients. A recent study from the Rockefeller University in New York and Prof Florian Klein, University Hospital Cologne and German Center for Infection Research (DZIF) has found an HIV neutralizing antibody effective against an HIV strains.
10-1074: The HIV Neutralizing Antibody
Scientists are optimistic about the newest generation of HIV neutralizing antibodies. Prof. Florian Klein and his team decided to test one of these antibodies. They wanted to find out if it could be used to treat the disease.
Prof. Klein states “These antibodies are highly potent and are able to effectively neutralize a large number of different HIV strains. Therefore, they play an important role in the quest for and development of an HIV vaccine.”
The 10-1074 antibody targets a certain structure on the HIV envelope protein. The antibody proved effect as a drug and antibody during testing. The results of this research saw a high antiviral activity within patients who have HIV.
Positive News
Through the collaborative work among the three institutions, this is positive news for patients with HIV. They are already looking at how the virus escapes most antibodies.
“We performed a comprehensive HIV sequence analysis to investigate the dynamics and mechanisms HIV uses to escape the selection pressure by the antibody,” says Dr. Henning Gruell, one of the first authors of the current publication.
HIV is still a troubling disease. By the end of 2015, there were 2.1 million newly infection patients with HIV and 36.7 million people living with the virus. More than 18.2 million are prescribed antiretroviral therapy. These numbers are startling.
The most important thing anyone can do in the fight against HIV is get tested. Knowing your status helps you take the rights steps to protect your health. Visit an HIV doctor today.