Posts tagged Antiretroviral drugs

Age Affects HIV Treatments in Individuals
HIV affects many people in the United States, and finding the right HIV treatments is difficult. A new article, published in the Journal of the American Geriatrics Society, suggests that age affects treatment for elderly patients. New age-specific strategies need to be developed to combat the virus.
Age and HIV
Unfortunately, a certain percentage of young people in America have contracted HIV. According to the CDC, in 2012, around 44% of young people around the age of 18 to 24 years old were living with HIV they did not know they had. Even more frightening is the fact that by 2014, young people around the age of 13 to 24 years old made up more than 1 in 5 new HIV diagnosis.
Meanwhile, the elderly are at risk too. Older adults aged 55 and older, account for at least 26% of the estimated 1.2 million people living with HIV. This group, in particular, is at a greater risk. They have the same risk factors as younger people, but they are less aware of what can cause HIV.
Developing Age-Specific HIV Treatments
Since many older adults are less aware of HIV risk factors, they have an increased risk for late or missed diagnosis. Even worse, they are more susceptible to disease, meaning drugs carry more side effects for them. Researchers began investigating based on the need for elderly patients to receive proper HIV treatments.
“Our article highlights the need for more research on screening, evaluation, and treatment in older adults infected with HIV. As the number of older people living with HIV grows, we need scientifically sound data to help prepare our clinicians and healthcare systems for the unique needs and expectations of this group,” said Dr. Aroonsiri Sangarlangkarn, co-author of the Journal of the American Geriatrics Society article.
Hopefully, physicians will see this research as a means to find better HIV treatments for older adults. Using the right tools can help with diagnosing these patients and helping them live with the disease.

Enlightening Effect of Observing HIV Cellular Transmission
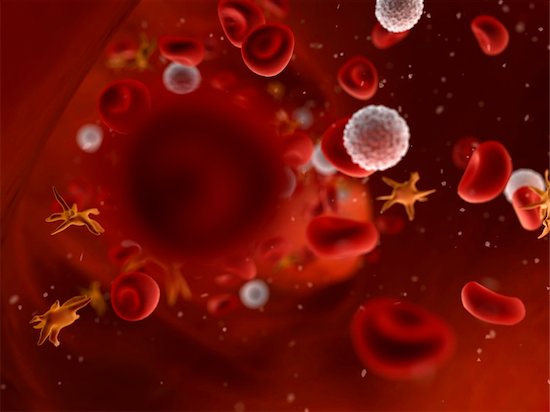
Scientists have discovered some interesting facts about the cellular transmission of HIV and how the virus moves throughout the body.
The inner workings of HIV, and the effectiveness with which it is able to transmit and spread infection, are complex. HIV cellular transmission has been carefully studied now for decades. The virus establishes itself in the host a couple of ways, and new information continues to be discovered. Cell-to-cell transmission has also been observed in the lab. Scientists have now been able to track HIV as it infects cells in real time in living organisms. This has big implications for the current approach to treatment and therapy.
Immune Cellular Transmission and the Role of Mutation
In this latest study, tracking HIV cellular transmission from cell to cell revealed a number of facts. First, the infected immune cell meets up with an uninfected cell, both being CD4 helper T cells. A sort of bridge is constructed between the two, and viral material that is passed along infects the second cell. The process, according to the researchers, is similar to the way nerve cells communicate information with each other. Cellular transmission works quickly. Several copies of the virus can pass through the bridge, making mutation easier. Mutant forms of the virus make it easy to escape detection from the immune system. This potent means of infection could prompt researchers to look to new approaches for treatment. Cell-to-cell transmission may increase resistance to antibodies, and the cells seem more resistant to current treatment options.
Today, antiretroviral therapies target viral particles floating in the bloodstream. It could be that cell-to-cell transmission takes place rapidly and goes undetected until the virus can be found in the blood. Reservoirs of infected cells are found in different tissues. Once infected, the immune cells can replicate, and clusters form rapidly. Treatments focusing on limiting or halting cell-to-cell transmission may be more effective at curbing the infection than current methods. Evidence that this could be useful if applied to potential vaccines was indicated as well.
In the U.S. alone, over one million people are living with HIV, and almost 40 million cases worldwide, so the search for effective treatments continues.

The Enzyme That Could Be Used Against HIV
HIV can now be managed as a chronic disease, largely due to modern antiviral medications. These medications target the enzyme, protease. Inhibiting the enzyme aids in preventing the infection from spreading within the body by slowing the maturing process. However, studies are now showing that the very enzyme that speeds up maturation can also destroy the virus if certain processes were to be delayed. This could mean that within a decade we will see a new generation of medications used to treat and manage HIV with potentially fewer side effects.
Halting the Spread by Activating the Enzyme Early
Once a cell is infected, a sort of bud forms from the cell. This sac-like structure contains viral particles that will soon become mature HIV. Once the bud is released, it is the protease enzyme that goes to work in order to morph the particles into a mature, infectious virus. Afterward, it floats around until a new, healthy cell is found and infected, thus starting the process over again. This then makes it understandable why the current therapies are aimed at stopping protease. Researchers have found, however, there are certain factors that, when changed, can cause the enzyme to activate prematurely. If this happens prior to the bud releasing from the host cell, it means the viral particles that were released will not be able to mature, and thus are not infectious.
When the protease activates before the bud releases, it causes a leak of proteins and enzymes into the host cell. Once the bud actually releases, there is no more enzyme to trigger the maturing phase. How does protease activate early? Everything works on the precise timing of events. The viral interaction with certain proteins is important to timing the release. Should an interaction be compromised, a delay can occur. The protease activates regardless of whether the bud has separated or not. With the release time delayed and the proteins gone, there is nothing left for the virus when the bud is finally detached, and it is rendered impotent.
Current medications can cause a spectrum of side effects that are often experienced. Therefore, many programs and studies are focusing on effective therapies with fewer side effects.
Link Between HIV and Zinc Deficiency
Living with HIV while on antiretroviral therapy usually means that an individual will have or will experience secondary conditions. Quality of life and overall life expectancy have continued to rise, yet there is room for improvement. This is especially the case when certain conditions can signal progression in the disease – such as zinc deficiency and inflammation.
Inflammation and HIV
Inflammation is an immune response that can become overactive with HIV treatment. Efforts to understand what causes this to happen, and how to reduce the inflammation, have been the focal point for a number of research projects around the world. One particular study linked a lack of zinc to higher rates of inflammation.
Zinc Deficiency and Inflammation
The study helped to link a deficiency in the nutrient zinc—a condition that is commonly found in those who are HIV-positive—and inflammation. Through a close examination of hundreds of patients with HIV who are on antiretroviral therapy, they were able to acquire information specific to this topic. Rigorous gathering of statistics, diet information, blood samples, interviews, and other samples was necessary to confirm the findings.
Certain biomarkers used to identify inflammation can be used to analyze the progression of the condition. One of those markers relates to zinc. The higher the concentration of the marker, the less zinc there was. This deficiency could help with gaining better control over the effects of the infection. If confirmed that this is the case, it could lead to relieving some symptoms from sufferers and improve quality of life. Scientists are also hoping that other groups would likewise benefit from these results.
More Questions About Zinc Deficiency Than Answers
While the link between the biomarker and the lack of zinc are clear, a few questions were raised. For one, researchers are not sure if the inflammation is caused or aided by the lack of zinc. It could be that zinc deficiency is the result of the inflammation. Along with these issues, there are some doubts that simply increasing zinc in one’s diet would help rectify the problem. In order to be conclusive, more information is needed.
HIV and HCV Co-Infection Creates Treatment Concerns
It is not uncommon for a person infected with HIV to also have a co-infection with the hepatitis C virus (HCV). Treatments for each infection are usually necessary. Ongoing research hopes to bring to light how to best treat each condition and keep the disease from progressing. Two recent studies presented conclusions that differed when it came to the effectiveness of certain treatments aimed at HCV.
Reports on Treating Co-Infection
The first report showed that when a person has both infections, HIV can slow the elimination or control of the hepatitis C infection. Those with only the HCV could be successfully treated, or at least lower the amount of the virus in the body after only a few months. When examining those with a co-infection of HIV, the results were different. In these patients, the HCV held on for a long period of time. This leads some to conclude that when both viruses are present, a new approach to treatment may be in order.
However, another recent study came up with different conclusions. This second study suggests that specific types of treatment can eliminate the need to worry about interference from the second infection. In the research done here, those with a co-infection of HIV and HCV were successfully treated for HCV. The specific pharmaceuticals used seemed as effective for those who had HIV as those who did not. The numbers for those with co-infections were similar to those with just the one. Different drugs were used in this study than in the other, so that may explain some of the discrepancies.
In conclusion, more information is needed. Current treatments for HCV do work; they may simply need some tweaking when HIV is present. When treating patients with both conditions, physicians do well to closely track progress and evaluate the effectiveness of such treatments. Adapting to a patient’s needs could go a long way in helping to eliminate the infection. In the meantime, researchers are working to resolve the issues brought to light. The results of the two studies do highlight the importance of finding answers in an effort to help more people.


