HIV Research

New HIV Neutralizing Antibody Proves Successful
It is always good news when scientists make brand-new developments in HIV research. Breakthrough information helps scientists and doctors create new medicine and therapies for patients. A recent study from the Rockefeller University in New York and Prof Florian Klein, University Hospital Cologne and German Center for Infection Research (DZIF) has found an HIV neutralizing antibody effective against an HIV strains.
10-1074: The HIV Neutralizing Antibody
Scientists are optimistic about the newest generation of HIV neutralizing antibodies. Prof. Florian Klein and his team decided to test one of these antibodies. They wanted to find out if it could be used to treat the disease.
Prof. Klein states “These antibodies are highly potent and are able to effectively neutralize a large number of different HIV strains. Therefore, they play an important role in the quest for and development of an HIV vaccine.”
The 10-1074 antibody targets a certain structure on the HIV envelope protein. The antibody proved effect as a drug and antibody during testing. The results of this research saw a high antiviral activity within patients who have HIV.
Positive News
Through the collaborative work among the three institutions, this is positive news for patients with HIV. They are already looking at how the virus escapes most antibodies.
“We performed a comprehensive HIV sequence analysis to investigate the dynamics and mechanisms HIV uses to escape the selection pressure by the antibody,” says Dr. Henning Gruell, one of the first authors of the current publication.
HIV is still a troubling disease. By the end of 2015, there were 2.1 million newly infection patients with HIV and 36.7 million people living with the virus. More than 18.2 million are prescribed antiretroviral therapy. These numbers are startling.
The most important thing anyone can do in the fight against HIV is get tested. Knowing your status helps you take the rights steps to protect your health. Visit an HIV doctor today.

HIV Breakthrough Deciphers the Structure of the Virus
There is one question that has eluded scientists for so many years. How does HIV integrate into human host DNA and replicate in the body? More than a decade later, researchers have found the answer. An HIV breakthrough at the Salk Institute has deciphered the structure of HIV machinery.
Intasome: The Machinery Making Trouble
HIV intasome is a large molecular machine that adds viral DNA into the genomes of its host. This machinery is responsible for HIV’s elusive nature and its ability to hide within the body.
According to Dmitry Lyumkis, senior author, and fellow at the Salk Institute: “HIV is a clever virus and has learned to evade even some of the best drugs on the market. Understanding the mechanisms of viral escape and developing more broadly applicable drugs will be a major direction in the future.”
Scientists have come up with a way to combat intasome before by using a drug called integrase strand transfer inhibitors (INSTIs). It is approved to treat the virus in both the U.S. and Europe. However, the drugs and HIV machinery are a bit of a conundrum. Without being able to study intasome on the atomic level, the drug’s effects are not as powerful as it should be, leaving scientist stumped on how it should work.
How This HIV Breakthrough Was Made
New technology allows us to do better things. The same is true within the scientific community. The state-of-the-art imaging technique called the single-particle cryo-electron microscopy (cryo-EM) gave researchers the ability to image large, complex and dynamic molecules. Basically, they were able to see intasome structure clearly.
The molecular machine is composed of a four-part core but has many other complex parts to it. The researchers believe that this allows it to gain access to the cell’s nucleus through active transport instead of waiting for the cell to divide. Lyumkis calls for understanding each of these parts a bit more to combat the disease.

HIV Vaccine Shows Promise in Preclinical Trial
The race to stop the spread of HIV continues. Despite the best efforts of doctors and researchers, new cases of the viral infection continue to crop up. That is why a preclinical trial is important. Halting this spread depends on finding solutions that work, and are also cost effective so as to be readily available in poorer countries. The urgency is more critical than ever before, yet there is the promise of effective vaccines, new treatments, and perhaps a cure someday. While the search for better treatments and cures is at its peak, an HIV vaccine option has emerged that has the scientific community buzzing. To date, it has proven successful in two preclinical trials.
A Second Preclinical Trial Confirms the Results
The HIV vaccine in question is designed to prevent infection obtained via mucosal membranes. Specifically, it has been tested both times in conditions that mimic male-to-female contact, with the male being the one infected and the female receiving the vaccine. A second line of defense that’s designed into the vaccine is to protect against infection by generating blood antibodies. A similar preclinical trial was first conducted in China, where results showed enough promise to warrant the study be done again, but on a slightly larger scale. It was this second study that produced excitement at the promise of a potential new vaccine. Just as the first study was successful, the second preclinical trial repeated those results. Even with repeated exposure to the virus, the vaccines were able to stave off infection. Not only that, each exposure was up to 100,000 times the normal dose of HIV passed from human to human.
What now? A component of the vaccine has been tried on human participants. This first phase of clinical trials yielded positive results, especially in regards to safety and tolerance. This particular vaccine has other benefits its designers implemented that give it global appeal. For instance, it will be tested and available in liquid form and needle-free. This is done with the goal of making it readily affordable to countries or areas with limited resources in order to reach as many as possible.

The Enzyme That Could Be Used Against HIV
HIV can now be managed as a chronic disease, largely due to modern antiviral medications. These medications target the enzyme, protease. Inhibiting the enzyme aids in preventing the infection from spreading within the body by slowing the maturing process. However, studies are now showing that the very enzyme that speeds up maturation can also destroy the virus if certain processes were to be delayed. This could mean that within a decade we will see a new generation of medications used to treat and manage HIV with potentially fewer side effects.
Halting the Spread by Activating the Enzyme Early
Once a cell is infected, a sort of bud forms from the cell. This sac-like structure contains viral particles that will soon become mature HIV. Once the bud is released, it is the protease enzyme that goes to work in order to morph the particles into a mature, infectious virus. Afterward, it floats around until a new, healthy cell is found and infected, thus starting the process over again. This then makes it understandable why the current therapies are aimed at stopping protease. Researchers have found, however, there are certain factors that, when changed, can cause the enzyme to activate prematurely. If this happens prior to the bud releasing from the host cell, it means the viral particles that were released will not be able to mature, and thus are not infectious.
When the protease activates before the bud releases, it causes a leak of proteins and enzymes into the host cell. Once the bud actually releases, there is no more enzyme to trigger the maturing phase. How does protease activate early? Everything works on the precise timing of events. The viral interaction with certain proteins is important to timing the release. Should an interaction be compromised, a delay can occur. The protease activates regardless of whether the bud has separated or not. With the release time delayed and the proteins gone, there is nothing left for the virus when the bud is finally detached, and it is rendered impotent.
Current medications can cause a spectrum of side effects that are often experienced. Therefore, many programs and studies are focusing on effective therapies with fewer side effects.

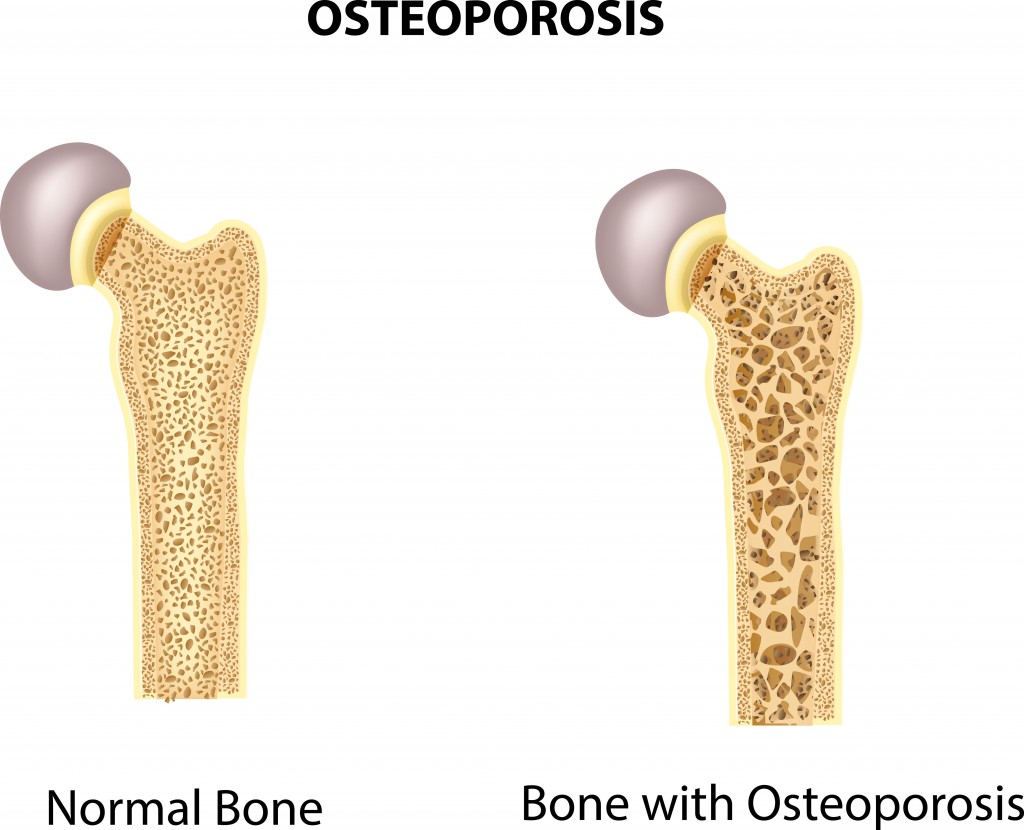
HIV and Bone Loss in Infected Young Men
Certain physiological occurrences are expected for patients who are infected with HIV. Bone loss is one of the effects that tops the list. It has been documented that those with the disease are more likely to present with fractures than someone who is not HIV-positive. High rates of osteoporosis and osteopenia are not new. However, recent research shows a discrepancy between the sexes in this matter. Further investigation revealed some information that could prove helpful for physicians as they treat HIV-positive individuals.
The most noticeable difference is the percentage of men versus the percentage of women who present with osteoporosis or osteopenia. Men actually have a much higher rate of the condition than women. It is estimated that 90% of HIV-infected men have bone loss while females with HIV come in around 60%.
HIV causes chronic inflammation due to disruption and dysfunction of the immune system. Antiretroviral therapies also add to the body’s burden of maintaining bone mass. These conditions are known to slowly erode bone. Studies show that in preteen and teenage males, there is an increase of what is called macrophages. These white blood cells, when found in the bone, are responsible for resorption during remodeling of the bone when it is continuous.
Predicting and Preventing Bone Loss
Digging a bit deeper, the more of these specialized cells there were, the less dense the bone material proved to be. If the production of the macrophages increases, it seems to indicate bone loss. It is hoped that with this information, newly infected patients can be watched for these types of changes, and thereby the amount of bone lost can be reduced.
For the feminine side, chronic inflammation generally is more prevalent in females. However, due to the presence of estrogen, the rate of bone loss is lessened. Estrogen acts as a shield against some of the inflammation. Estrogen is also effective at blocking the production of macrophages. These two properties together seem to account for the lower figures of bone loss in females when compared to males.