The Progression of HIV: How the Infection Takes Over Your Body
It’s important to know every aspect of HIV, in particular for those infected with the virus. HIV is a volatile disease and an epidemic that has claimed the lives of over 35 million people. Understanding how the disease works can help patients make better decisions when it concerns their health. That’s why it’s imperative that patients are informed because over time and without proper treatment, HIV develops into something much worse. Find out everything you need to know about the progression of HIV and how you can protect yourself.
Laying Out the Progression of HIV
HIV progresses in three stages. As the disease moves from one stage to the next, it becomes worse over time. Eventually, the disease completely eradicates the immune system, leaving the body vulnerable to other diseases and infections. Let’s walk through the different stages of the virus and what it means for HIV-positive individuals.
Stage 1: Acute HIV Infection
The progression of HIV starts soon after infection. The first stage of the virus is known as acute HIV infection. During this stage, symptoms aren’t noticeably apparent, and for the first 2 to 4 weeks, people may be unaware that they have contracted the disease. There is a chance that HIV-positive individuals experience flu-like symptoms. These symptoms are a telling sign for anyone who has recently participated in risky sexual activity or drug use. It usually means that they have contracted the virus and it has start to multiply, causing it to spread within the body and destroy the immune system.
Stage 2: Clinical Latency
As defined by the CDC, Clinical Latency is the second stage of the virus. It is also known as asymptomatic or chronic HIV infection. While still active within the body, the HIV virus reproduces at low levels. Most people still do not show any symptoms of the disease by this point. However, it is important to note that one can still spread the infection to others. This stage is also a crucial period as the disease can evolve and become AIDS without proper treatment.
Stage 3: AIDS
AIDS is the final stage of HIV. This is when the number of CD4 cells in the body, which aid the immune system, are at their lowest. AIDS grants other infections and diseases the opportunity to damage the body severely. Your symptoms often depend on the type of illness or opportunistic infection you contract. This stage can occur when one has not properly taken medication during the first or second stage of the virus. Patients with AIDS who continue to ignore treatments usually live for three years.
Slowing Down the HIV Infection
While there is no cure for HIV, scientists are working diligently every day to find one. Their research has led to advancements in HIV medications. By taking this treatment, patients can slow the progress of the disease. Some have even found success in keeping it at stage 2 for many years, preventing the transition to AIDS. For this treatment to be effective, patients must take the antiretroviral medications every day. If you are worried or concerned that you may have contracted HIV, contact an HIV specialist today and get tested as soon as possible.

The Sneaky Nature of the HIV Virus
There is no doubt that HIV is a deadly virus. Since it was discovered, this pandemic has infected 78 million people and 35 million have died due to an AIDS-related illness. The worst part is that scientists have yet to find an absolute cure to the disease. Why is it that the HIV virus is so hard to eradicate? What is it about the disease that makes treatment difficult?
Many experts note the infection’s ability to hide within the body. HIV is notorious for eluding even the most powerful combinations of medicine. The sneaky nature of the disease allows it to wait until the right moment, when the body’s defenses are down, to attack the immune system. Even today, scientists are still trying to figure out and understand exactly how the virus works in order to combat its effects on the body.
How the HIV Virus Moves Within the Body
Once the body is infected with HIV, the virus begins to attack the immune system. It’s number one target are the CD4 cells in the body. These cells help the immune system fight off infection and diseases. Little by little, HIV lowers the CD4 count until the body can no longer protect itself.
The best defense against HIV is antiretroviral therapy (ART). This is a combination of several medications that work together to suppress HIV levels in the body. In order for this treatment to work, it has to be taken daily. When taken properly, the treatment has proven effective in reducing traces of the virus to nearly undetectable levels and preventing the progression of the disease to aids.
What Studies Have Found
ART is no cure. Traces of the virus remain within the body despite the use of these strong medications. The virus likes to hide in immune cells when at low levels. By remaining dormant in these “Sanctuary Sites,” it can wait in places unreachable by drugs. Once it has found the right moment, it will quickly reproduce when an HIV positive individual stops taking ART therapy.
In a recent joint study by the Monash Biomedicine Discovery Institute and the Systems Immunity Research Institute at Cardiff University, the two institutions discovered that mutations within HIV help it appear dormant and virtually undetectable by the immune system. These mutations change the way that key immune molecules called Major Histocompatibility Complex (MHC), display the virus.
“This work uncovers a novel mechanism for HIV immune escape, which will be important to incorporate into future vaccine development and may have broader implications for immune recognition of MHC molecules,” he said.
What You Can Do
While scientists work hard to find a way to detect and eradicate the HIV virus completely, you have to do your part to curb the spread of the virus. Protect by getting tested. Knowing is an important step. If you are HIV-negative, protect yourself by practicing safe sex and taking pre-exposure prophylaxis (PrEP). For those infected by the disease, remember to take ART daily to prevent the virus from progressing.

Early HIV Intervention Helps Manage HIV-Like Virus
Nothing is more important than getting tested for HIV as soon as possible. If you test positive, an early diagnosis can increase your chances of managing the virus. Early HIV intervention is a crucial step in protecting your health. HIV can be a tricky disease that likes to hide. This makes the virus difficult to treat before it attacks the immune system.
In a study to better control the disease’s progression within the body, the Rockefeller University tested and treated monkeys infected with an HIV-like virus. Find out the results of their research and what this could mean for patients with HIV.
New Form of HIV Therapy
The Rockefeller University and the National Institute of Health wanted to find a way to tackle HIV while it lays dormant within the body. The virus often hides like this to avoid being eradicated. It waits for the perfect opportunity, like when treatment is interrupted, to attack the immune system.
Using macaque monkeys and a model of HIV, the researchers were able to simulate the effects of the HIV virus in humans. 13 monkeys were tested over a two-week period of they were injected with the virus. While the model, which is known as the simian-human immunodeficiency (SHIV), is not a 1 to 1 recreation of the virus, it helps explore ways to control the virus.
The new treatment uses two anti-HIV antibodies to give a boost to the immune system. These antibodies were discovered in individuals with a rare ability to fight the infection. New drugs (3BNC117 and 10-1074) were developed and they enable the body to take control of the virus and hold off its effect for a long period of time. However, the researchers suggest that this all works because the treatment was given soon after infection.
“This form of therapy can induce potent immunity to HIV, allowing the host to control the infection,” says Michel Nussenzweig, head of the Laboratory of Molecular Immunology and an Investigator with the Howard Hughes Medical Institute. “It works by taking advantage of the immune system’s natural defenses, similar to what happens in some forms of cancer immunotherapy.”
The Success of Early HIV Intervention
The monkeys showed significant improvement after taking the new drugs. After treatment was initially given, HIV levels dropped until they were nearly undetectable. The positive progress of the subjects continued 5 to 22 months later as the monkey regained control of the virus. The virus then dropped again and stay at low levels for another 5 to 13 months.
Further studies need to be done to see if this treatment is feasible in humans. During the study, the scientists also investigated cytotoxic T cells. When they decreased these cells in the monkeys’ bodies, SHIV levels increased. It proved that these cells may have helped the monkeys fight off the virus.
Their next test is to see if the drugs are still effective after long-term infection and without early HIV intervention. They are going to have the monkey exposed to the virus for about two to six weeks before treating them. Hopefully, the results will remain positive.

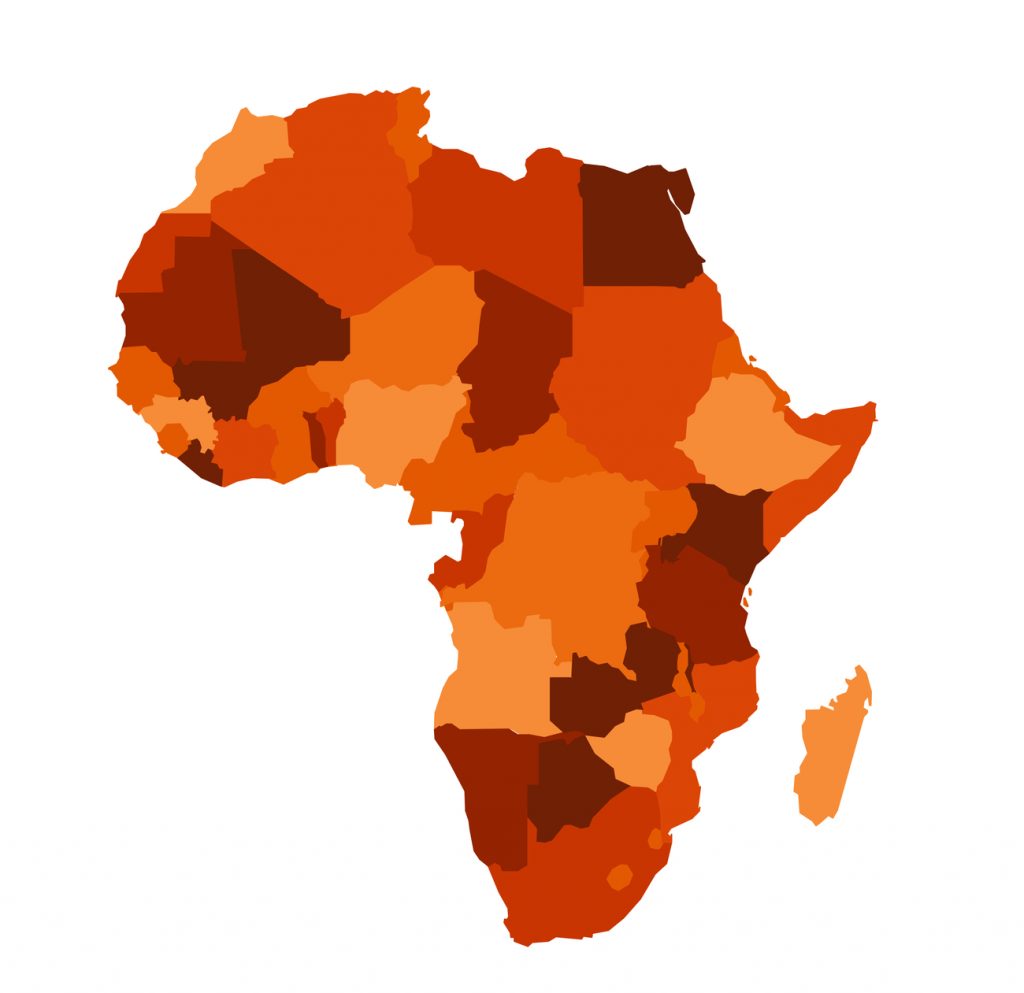
Hypertension an Increasing Problem for Africans Living With HIV
HIV is a worldwide epidemic. From country to country, the virus has a significant impact. This makes it harder to provide the resources to fight against the virus. In sub-Saharan Africa, there were 24.7 million people living with HIV in 2013. Even worse, the number of new HIV infections are up to 1.5 million. Only 39% of adults receive antiretroviral treatment.
At-Risk Individuals
There are several key groups affected by HIV within this region of the world. Unfortunately, research has shown that many of the countries in Africa, mainly Southern Africa, are the worst affected by the disease. The government continues to encourage and offer more testing for the population but many individuals are unaware of their status, leaving the country at continued risk.
The groups who are the most at risk included young women, children, sex workers, men who have sex with men, and drug users. There are several factors putting these groups in danger. Condom distribution varies from country to country. It is also not uncommon to find younger women in relationships with older men. More than 4 in 10 new infections are young women around the 15-24, who are participating in unsafe sexual behavior.
Hypertension and Living With HIV
A new problem has risen in the region of sub-Saharan Africa. Scientists are discovering a high prevalence of hypertension among rural Africans. New research reveals that about 12 percent of people living with HIV in Tanzania have hypertension when they are diagnosed. Furthermore, an additional 10 percent of the population will develop Hypertension during the first months of antiretroviral therapy.
Tanzania has approximately 1.4 million people living with the virus. However, the country has done well to curb the spread of disease. New infection dropped by more than 20% between the years of 2010 and 2015. This is due in part to the increase of antiretroviral drugs in the area.
The researchers note that the development of hypertension in these patients is likely in relations to normal cardiological risk factors like age, body mass index, and renal function. The effect that antiretroviral drugs have on the body may play a role, though.
How Scientists Plan to Address the Issue
The prevalence of HIV and hypertension is 1.5 times higher than both Europe and the United States. This is trouble for a region that is already dealing with this epidemic. Dr. Emilio Letang, Swiss TPH and Barcelona Institute for Global Health (ISGlobal) has a few suggestions to combat the combination of both conditions.
“We have seen that such routine screening is a feasible and effective strategy to diagnose hypertension within an HIV programme. Moving forward, however, we need to make sure that leveraging such synergies does not compromise the efficiency of existing HIV programmes,” says Dr. Emilio.
Prof. Dr. Christoph Hatz, Chief Medical Officer at Swiss TPH continues by stating that “In many countries across sub-Saharan Africa, there is still a lack of access to drugs against major non-communicable diseases. In order for such integrated care programmes to work successfully, ensuring better availability and affordability of drugs as well as implementing comprehensive preventive and curative measures will be key.”

Computer Analyzes Adverse HIV Drug Effects
Drugs are often a double-edged sword. While their purpose is to cure or alleviate symptoms caused, many of them come with complications. This is often the case with drugs for severe conditions such as HIV drugs.
Furthermore, HIV is one of the most troublesome diseases in the world. Medications help fight off the virus but they can also have adverse effects on the body. One of the most common drugs for HIV is abacavir. The side effects of this drug are rare but a certain portion (5 to 8 percent) of patients do experience an intense allergic reaction to it.
Abacavir is known to cause hypersensitivity syndrome. This is a life threating reaction which can cause fever, rash, nausea, vomiting, diarrhea, and abdominal pain. If patients have a particular human leukocyte antigen (HLA), these symptoms usually appear within the first two to six weeks of taking the HIV drug.
The HLA protein is a substance that induces an immune response. These proteins are located on the surface of a cell and often communicate with T-cells. If an entity other than a co-binding peptide binds to an HLA protein and changes it, the protein will deem it foreign. This signals the T-cells, and cause an immune response. Often, the abacavir drug appears as an unknown entity when it tries to bind to the cells.
Researchers Take a Closer Look at HIV Drug
A test was performed at North Carolina State University. Researchers used a computer model to get a closer look at the abacavir drug reaction on a molecular level. They wanted to see the drug’s interaction with the HLA proteins.
“There are 15,000 variants of HLA, and everyone carries some of these variants,” says Denis Fourches, assistant professor of chemistry at NC State. “HLA-B*57:01 is one of the first variants studied in the context of a drug-induced immune reaction. We know that it binds with abacavir, but little was understood about exactly what was happening structurally at the molecular level, especially in terms of the relationship with the co-binding peptide. This is a very complex system.”
The computer was able to create 3D models of the HLA protein, abacavir, and the co-binding peptides. Researchers simulated the docking process with and without co-binding peptides. They also ran simulations of the process with 13 other HIV drugs that have similar effects.
“The models allowed us to identify key atomic interactions that cause abacavir and other drugs to bind to the HLA variant protein and ultimately trigger the immune response,” Fourches says. “When you can forecast and understand the elements of the drug that enable the binding to occur, you may be able to create new active compounds that do not have that problem.”
The research team at NC state hopes that his in-depth look at binding process will provide them a better understanding of how the immune system reacts to drugs. With this knowledge, they can predict the side effects of medications. In the future, they can also build better drugs. Hopefully, they will avoid life-threatening situations.