Posts tagged HIV/AIDS

Enlightening Effect of Observing HIV Cellular Transmission
Scientists have discovered some interesting facts about the cellular transmission of HIV and how the virus moves throughout the body.
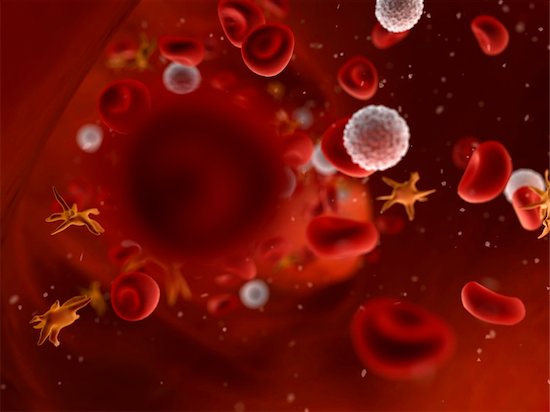
The inner workings of HIV, and the effectiveness with which it is able to transmit and spread infection, are complex. HIV cellular transmission has been carefully studied now for decades. The virus establishes itself in the host a couple of ways, and new information continues to be discovered. Cell-to-cell transmission has also been observed in the lab. Scientists have now been able to track HIV as it infects cells in real time in living organisms. This has big implications for the current approach to treatment and therapy.
Immune Cellular Transmission and the Role of Mutation
In this latest study, tracking HIV cellular transmission from cell to cell revealed a number of facts. First, the infected immune cell meets up with an uninfected cell, both being CD4 helper T cells. A sort of bridge is constructed between the two, and viral material that is passed along infects the second cell. The process, according to the researchers, is similar to the way nerve cells communicate information with each other. Cellular transmission works quickly. Several copies of the virus can pass through the bridge, making mutation easier. Mutant forms of the virus make it easy to escape detection from the immune system. This potent means of infection could prompt researchers to look to new approaches for treatment. Cell-to-cell transmission may increase resistance to antibodies, and the cells seem more resistant to current treatment options.
Today, antiretroviral therapies target viral particles floating in the bloodstream. It could be that cell-to-cell transmission takes place rapidly and goes undetected until the virus can be found in the blood. Reservoirs of infected cells are found in different tissues. Once infected, the immune cells can replicate, and clusters form rapidly. Treatments focusing on limiting or halting cell-to-cell transmission may be more effective at curbing the infection than current methods. Evidence that this could be useful if applied to potential vaccines was indicated as well.
In the U.S. alone, over one million people are living with HIV, and almost 40 million cases worldwide, so the search for effective treatments continues.

The Enzyme That Could Be Used Against HIV
HIV can now be managed as a chronic disease, largely due to modern antiviral medications. These medications target the enzyme, protease. Inhibiting the enzyme aids in preventing the infection from spreading within the body by slowing the maturing process. However, studies are now showing that the very enzyme that speeds up maturation can also destroy the virus if certain processes were to be delayed. This could mean that within a decade we will see a new generation of medications used to treat and manage HIV with potentially fewer side effects.
Halting the Spread by Activating the Enzyme Early
Once a cell is infected, a sort of bud forms from the cell. This sac-like structure contains viral particles that will soon become mature HIV. Once the bud is released, it is the protease enzyme that goes to work in order to morph the particles into a mature, infectious virus. Afterward, it floats around until a new, healthy cell is found and infected, thus starting the process over again. This then makes it understandable why the current therapies are aimed at stopping protease. Researchers have found, however, there are certain factors that, when changed, can cause the enzyme to activate prematurely. If this happens prior to the bud releasing from the host cell, it means the viral particles that were released will not be able to mature, and thus are not infectious.
When the protease activates before the bud releases, it causes a leak of proteins and enzymes into the host cell. Once the bud actually releases, there is no more enzyme to trigger the maturing phase. How does protease activate early? Everything works on the precise timing of events. The viral interaction with certain proteins is important to timing the release. Should an interaction be compromised, a delay can occur. The protease activates regardless of whether the bud has separated or not. With the release time delayed and the proteins gone, there is nothing left for the virus when the bud is finally detached, and it is rendered impotent.
Current medications can cause a spectrum of side effects that are often experienced. Therefore, many programs and studies are focusing on effective therapies with fewer side effects.

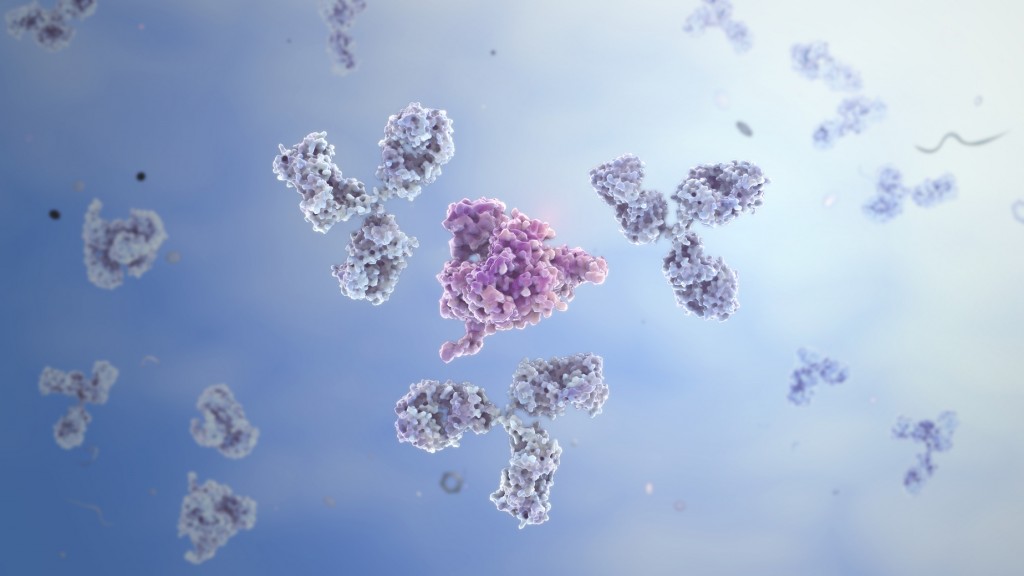
Using Antibodies in an Attempt to Find a Vaccine
The human immune system is a fascinating network capable of performing incredible feats. Even when HIV is involved, nearly one-third of individuals are capable of producing effective antibodies against the virus. Researchers have turned their attention to the antibodies produced during infection in order to facilitate the creation of an effective vaccine.
While some immune systems are adept at producing antibodies that act to neutralize a broad range of HIV strains, the process could, and often does, take up to a year before it is in full swing. Ideally, a vaccine should help a patient immediately combat the viral intrusion. This is one important goal for those developing vaccines. Efforts to speed up the process and make the antibodies available for everyone has prompted scientific study.
Certain effective antibodies were selected and closely examined. Of those, some had loop-like structures which, when they encountered the virus, were able to cling tightly and neutralize it. With the aid of computer modeling, modifications were made to the existing antibodies so as to maximize their efficiency. It is expected that such modifying will help increase the response time of the immune system, even if a person has never previously had contact with HIV.
Amino Acids Within Antibodies
Another aspect that was carefully reviewed was how the amino acids were sequenced in the antibodies that had proven most effective. Of the antibodies with a loop structure, certain ones had specific amino acid sequences that researchers tested and noted. A successful vaccine needs to provide adequate protection against more than just one or two strains of the tenacious virus. Those that were able to neutralize more strains were again plugged into the computer and modified. The re-engineering was to increase the capabilities of these powerhouse molecules.
Tests were also conducted to confirm that the alterations being made would, in fact, prove effective. The spectrum that the vaccine is designed to cover is wide, and when factoring in the potency of the design, researchers feel confident that if implemented, most people who are vaccinated would produce an effective response.

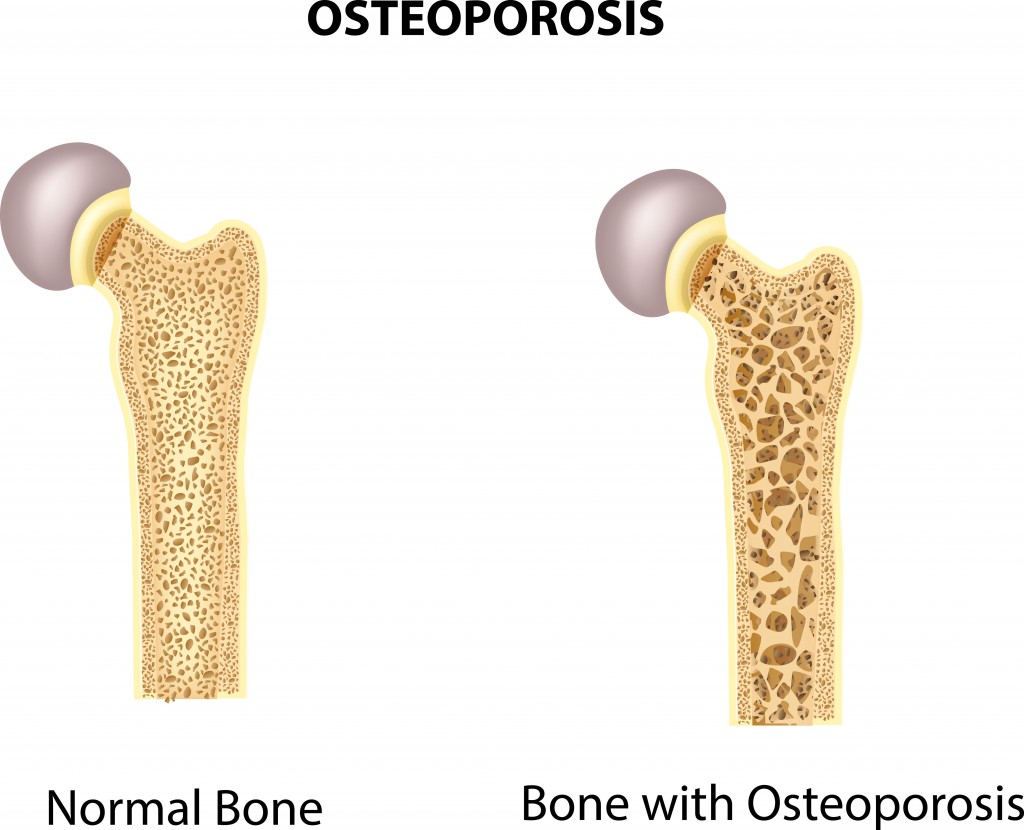
HIV and Bone Loss in Infected Young Men
Certain physiological occurrences are expected for patients who are infected with HIV. Bone loss is one of the effects that tops the list. It has been documented that those with the disease are more likely to present with fractures than someone who is not HIV-positive. High rates of osteoporosis and osteopenia are not new. However, recent research shows a discrepancy between the sexes in this matter. Further investigation revealed some information that could prove helpful for physicians as they treat HIV-positive individuals.
The most noticeable difference is the percentage of men versus the percentage of women who present with osteoporosis or osteopenia. Men actually have a much higher rate of the condition than women. It is estimated that 90% of HIV-infected men have bone loss while females with HIV come in around 60%.
HIV causes chronic inflammation due to disruption and dysfunction of the immune system. Antiretroviral therapies also add to the body’s burden of maintaining bone mass. These conditions are known to slowly erode bone. Studies show that in preteen and teenage males, there is an increase of what is called macrophages. These white blood cells, when found in the bone, are responsible for resorption during remodeling of the bone when it is continuous.
Predicting and Preventing Bone Loss
Digging a bit deeper, the more of these specialized cells there were, the less dense the bone material proved to be. If the production of the macrophages increases, it seems to indicate bone loss. It is hoped that with this information, newly infected patients can be watched for these types of changes, and thereby the amount of bone lost can be reduced.
For the feminine side, chronic inflammation generally is more prevalent in females. However, due to the presence of estrogen, the rate of bone loss is lessened. Estrogen acts as a shield against some of the inflammation. Estrogen is also effective at blocking the production of macrophages. These two properties together seem to account for the lower figures of bone loss in females when compared to males.
Link Between HIV and Zinc Deficiency
Living with HIV while on antiretroviral therapy usually means that an individual will have or will experience secondary conditions. Quality of life and overall life expectancy have continued to rise, yet there is room for improvement. This is especially the case when certain conditions can signal progression in the disease – such as zinc deficiency and inflammation.
Inflammation and HIV
Inflammation is an immune response that can become overactive with HIV treatment. Efforts to understand what causes this to happen, and how to reduce the inflammation, have been the focal point for a number of research projects around the world. One particular study linked a lack of zinc to higher rates of inflammation.
Zinc Deficiency and Inflammation
The study helped to link a deficiency in the nutrient zinc—a condition that is commonly found in those who are HIV-positive—and inflammation. Through a close examination of hundreds of patients with HIV who are on antiretroviral therapy, they were able to acquire information specific to this topic. Rigorous gathering of statistics, diet information, blood samples, interviews, and other samples was necessary to confirm the findings.
Certain biomarkers used to identify inflammation can be used to analyze the progression of the condition. One of those markers relates to zinc. The higher the concentration of the marker, the less zinc there was. This deficiency could help with gaining better control over the effects of the infection. If confirmed that this is the case, it could lead to relieving some symptoms from sufferers and improve quality of life. Scientists are also hoping that other groups would likewise benefit from these results.
More Questions About Zinc Deficiency Than Answers
While the link between the biomarker and the lack of zinc are clear, a few questions were raised. For one, researchers are not sure if the inflammation is caused or aided by the lack of zinc. It could be that zinc deficiency is the result of the inflammation. Along with these issues, there are some doubts that simply increasing zinc in one’s diet would help rectify the problem. In order to be conclusive, more information is needed.